Image by: KEVIN SUTHERLAND/EPA
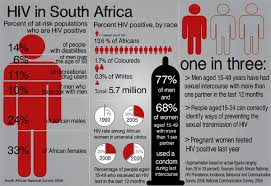
More than half a million South Africans contracted HIV last year.
Although South Africa had recorded a slight decline – about 0.03% – in the average number of infections between 2005 and 2015, hundreds of thousands of people are still being infected each year, according to a report released yesterday by the Global Burden of Disease collaborative network.
The estimated 529,670 infections in South Africa last year is the highest number in the world – compared with 104,200 in Zimbabwe and 196,600 in India. This country is one of six that have more than 10% of their population afflicted by HIV/Aids. The others are Lesotho, Namibia, Swaziland, Botswana and Zimbabwe.
The report, released at the 21st International Aids Conference in Durban, estimates that about 8.4million South Africans had HIV and about 155,000 died from Aids last year.
The findings were made public at a time when a worsening cash funding crisis is hobbling the fight against the disease. It was revealed at another HIV/Aids event yesterday that global funding of efforts to fight the disease had fallen by $1.1-billion (about R15.8-billion) between 2014 and last year – the first time global funding had decreased since 2010.
Charles Wiysonge, of the University of Stellenbosch, who collaborated on the Global Burden of Disease study, said there had been “a spike” of new infections in South Africa shortly after 2005, but this was being brought under control.
“We’re definitely better off than we were in 2005. We have rolled out antiretroviral drugs. There are 8.4 million people living with HIV in this country [and] this would have overwhelmed many countries. We are almost eradicating mother-to-child transmissions.
“We are doing very well … but there is no reason we should be seeing half a million new infections. That tells us that we are not doing as well as we should be doing,” he said.
A lot of the new infections, he said, had been in the 15-24 age group – particularly girls.
“We have a spike there, but not only there. We need to do a lot,” said Wiysonge.
Health Department deputy director Yogan Pillay said the numbers provided by Global Burden of Disease were higher than those derived from other studies and needed investigation.
“The estimates from the GBD [report] are significantly different, much higher [than those derived from] the Thembisa model of Leigh Johnson and UNAids. I need to study the assumptions in their model before I can comment substantively,” said Pillay.
“I can only guess at this stage that the model does not take into account the extent to which ARV coverage lowers new infections at a population level.”
South Africa was not the worst-hit country in respect of infections between 2005 and 2015. Seventy-four countries experienced an increase in infections. Worst hit were Pakistan (17.6% increase), Panama (13.6%), Qatar (13.06%) and Afghanistan (11%). Reasons for the rise in infections varied from country to country.
The increases, said the lead author of the Global Burden of Disease report, Haidong Wang, showed that the world had a long way to go before ridding itself of the disease.
“It has become quite evident to me, and it should be quite evident to the health community, that we face significant challenges in meeting the goal for the world to witness the end of Aids in less than 15 years,” he said.
He said there had been about 2.5million infections a year since 2005.
Peter Piot, founding director of UNAids and director of the London School of Hygiene and Tropical Medicine, said the findings were deeply worrying.
“The continuing high level of HIV infection is probably the most disturbing fact announced at the conference. It means that Aids is not over,” he said.
“The decline in international funding for the HIV response is worrying,” said Luiz Loures, UNAids deputy executive director. “Countries need urgent support over the next few years to fast-track their responses to HIV, enabling them to end the epidemic by 2030 and save millions of lives.”
HIV vaccine put on trial – Katharine Child
Young women in South Africa have among the highest rates of new infections in the world, but scientists are optimistic that South Africa is on track to roll-out a partially effective vaccine in about five years time.
The vaccine will be tested on 5700-HIV negative South Africans, aged 18 to 35, from November.
If the vaccine reduces the risk of contracting HIV by 50%, it will meet the licencing requirements needed by the Medicines Control Council to be brought to market. This was announced by the Head of the Medical Research Council Professor Glenda Gray on Tuesday. She is leading the trial.
While many vaccines offer 100% protection, Gray said modelling studies had shown that even a 50% reduced risk of contracting HIV would significantly drop the number of new infections in the country.
Gray said: “Our first prize is to roll it [ the vaccine] out in a school-based programme….. We think the most bang for your buck is to target young girls before they sexually debut and create a five- year blanket protection for them as they ….navigate the blessers of country.”
Gray said: “A vaccine is the ultimate female empowerment technology. You put it in a girl’s arm and you get protection in their vagina.”
Scientists have been searching for a prevention method to help South African young women who at huge risk of HIV.
Men can get circumcised to reduce their risk of getting HIV by 60% and often have the choice on whether to use a condom or not.
Scientists are cautiously optimistic the vaccine will come to market, because when it was first used in a trial in Thailand it reduced the risk of contracting HIV by 60% for the first year after use.
This waned to 31% protection after three years in the Thai people.
The vaccine being tested in South Africa in November has been boosted to be stronger and last longer than in Thailand.
Initial test results on 100 South Africans showed it worked better than expected – which is giving scientists optimism they may have something to protect women in a few years time.
http://www.timeslive.co.za/thetimes/2016/07/20/New-HIV-infection-topped-500000-in-SA-last-year