Hunger is still killing South Africa’s children

About 53 children under the age of five die in South Africa every day — and three-quarters of them do not live to see their first birthday.
Most of these children die of preventable causes — with malnutrition a key driver of under-five mortality in South Africa. A total of 31% of children who died in hospital between 2012 and 2013 were severely malnourished and a further 30% were underweight for their age.
But malnutrition doesn’t only threaten children’s survival, it undermines their ability to thrive and achieve their full potential.
Last year’s South African Demographic Health Survey found that 27% of children under five were stunted. This is a sign of chronic malnutrition that compromises not only children’s growth but also their cognitive development, education and employment chances.
These losses in human potential cost the country an estimated R62‑billion a year — and contribute to an intergenerational cycle of poverty and deprivation.
Yet despite this national crisis, the total dedicated allocation for nutrition amounted to only 0.5% of the primary healthcare budget for the period 2013-2014 to 2018-2019.
The immediate causes of malnutrition are linked to inadequate dietary intake and infection. Breastfeeding is the single most effective intervention for reducing childhood morbidity and mortality, yet only 24% of South Africa’s babies are exclusively breastfed at four to five months of age.
Greater commitment to, and investment in, community-based breastfeeding support is needed. We also need more support for working mothers — for example, maternity leave and breaks to allow them to breastfeed or express milk as mandated by the Basic Conditions of Employment Act, to ensure breastfeeding is sustained.
Given the legacy of apartheid spatial planning, childcare facilities should be provided at large workplaces to allow for breastfeeding by women who work far from home.
It is also vital to identify and support at-risk children whose growth is faltering before they need to be hospitalised. This includes using the health department-issued Road to Health booklet to monitor children’s growth effectively.
The failure of clinics and outpatient units to identify and timeously refer children with impaired growth (including moderate and severe malnutrition) is one of the key causes of child mortality that can — and should be — addressed. And failure to recognise other danger signs, coupled with the long distances many parents have to travel to clinics, may lead to further life-threatening delays in obtaining care.
Growth-promoting activities need to extend beyond simply weighing a child and plotting their growth to ensuring that hungry or malnourished children are linked to food provision, community health services and social assistance.
Greater investment is needed to scale up community-based services, as community health workers have proven effective in extending the reach of healthcare services to vulnerable households, promoting breastfeeding and nutritious weaning foods, and enabling the early recognition and treatment of acute childhood illnesses.
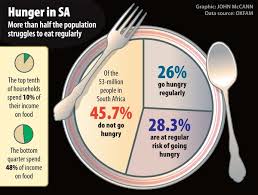
But the fundamental causes of malnutrition lie outside the healthcare sector. Poverty and unemployment continue to undermine household food security: 62% of children live in households with a monthly income of less than R965 a person. And, according to the 2016 Community Survey, 20% of households ran out of money for food in the past year — that is, one in five households. It is therefore not surprising that only 23% of infants aged six to 23 months have the minimum acceptable diet.
Unemployment is rising and young women of childbearing age are hardest hit — with 60% of 20- to 24-year-old women unemployed. The child support grant provides some relief and better nutritional outcomes — but, at R380 a month or little more than R12 a day, it fails to cover the nutritional needs of a child.
It is also failing to keep pace with food price inflation. According to the Pietermaritzburg Agency for Community Social Action, the costs of a basic food basket increased by 15% — and maize meal by 32% — between September 2015 and 2016. Yet the child support grant increased by only 6% over the same period. This gap is likely to widen in the current economic recession.
Finally, limited access to clean water and decent sanitation increases the risk of infection, especially in undernourished children: despite improved access, 24% of children under six still live in households without adequate sanitation and 32% without water on site.
The South African state is failing its children. It is unacceptable that children should go hungry and be denied their full potential in an upper-middle-income country with a Bill of Rights that places a high value on children’s rights.
Strong leadership and concerted intersectoral action are essential if we are to address the root causes of stunting, and so promote children’s optimal development and unlock South Africa’s human potential.
The fact that these are — to a significant extent — either absent or weak highlights the importance of civil society. It is urgent that child health advocates come together and establish a broad social movement for child health.
David Sanders, Louis Reynolds and Lori Lake are contributors to the South African Child Gauge 2017, released this week by the University of Cape Town’s Children’s Institute and partners. The 2017 issue explores how investing in children to ensure that they thrive and achieve their full potential will help to realise the development goals. It is available at ci.uct.ac.za See “Policy cannot disrupt food production”
https://mg.co.za/article/2017-12-01-00-hunger-is-still-killing-south-africas-children